 loading
loading
featuresBy reason of insanityA Yale Law alumnus, once hospitalized for schizophrenia, sues the state that detained him. Carole Bass ’83, ’97MSL, is senior writer at the Yale Alumni Magazine. 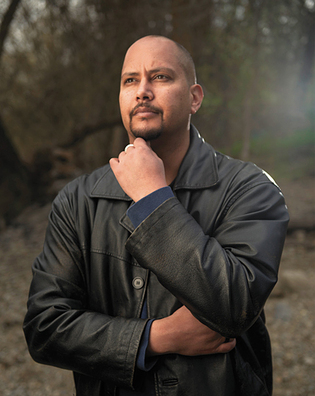 Matt LeitholtKetema Ross ’03Law committed violence in 2007 and was hospitalized. He says Washington State's treatment of patients like him, who need a court order just to walk the hospital grounds, is too harsh. View full imageKetema Ross came to Yale with a dream of changing the world as a civil rights lawyer. But during his first year as a law student, Ross lost his faith in the law as a tool for social justice. He also lost his grip on reality. The State Department started AIDS as a plot against black people, Ross told a friend that winter. By the summer, he believed the CIA was tapping his brain with a satellite. In his third semester, immediately after 9/11, he attended a single class, then withdrew and dropped out of sight, eventually returning to his hometown of Pullman, Washington. Early one morning in 2007, Ross heard President George W. Bush ’68 telling him that his next-door neighbors were traitors who needed to be gotten rid of. Ross broke into the elderly couple’s apartment and beat them with a broom handle. (They both survived the attack.) Charged with assault, he pleaded not guilty by reason of insanity. Now Ross says he has recovered his sanity, and a court order says he is no longer “a substantial danger.” And, after seven years of confinement in a psychiatric hospital, he has regained his freedom, mostly: by court order, he was conditionally discharged on January 11. What’s more, Ross has recovered some of his belief in the power of lawyers and the law to make the world a better place. With that renewed faith in civil rights law, he has teamed up with Yale College alumnus Andrew Biviano> ’97 on a federal lawsuit challenging Washington State’s approach to patients like him. The state’s approach to those found not guilty by reason of insanity, a 2014 report concluded, is unusually harsh. Patients are confined to a locked ward. They need a court order even to walk the hospital grounds, let alone to take supervised therapeutic outings. They can be held in the hospital indefinitely. Ross and Biviano believe this approach is grounded in fear, ignorance, and stigma. It turns patients into prisoners, they argue—often for far longer than people actually sentenced as felons for similar offenses. Ross says he could have accepted a plea bargain and been out of prison in three years—less than half the time he spent confined in the hospital. The suit, Ross v. Inslee, is a collaboration between two Yalies, with Ross the lead plaintiff and Biviano the lead attorney. Ross has made the unusual decision to put himself in the public eye as a person with mental illness. He is using his full name rather than a pseudonym or initials in the federal lawsuit; he’s granting interviews, with photos of himself; he appeared in a video on YouTube and has former law school classmates helping to publicize the cause. Ross has also done months of research, recruited other patients to join the suit as plaintiffs, and helped draft a complaint, according to Biviano. Biviano adds that Ross “recognized that he has to be the one to do this. He’s so intelligent and articulate that he’s much more persuasive than any legal arguments I can make.” Because Ross’s discharge is, so far, conditional, the lawsuit could affect how the hospital treats him. But he has other motives. “I’m doing it for the patients who’ve been here 10, 20, 30 years and have no hope” of being discharged, Ross said in a phone interview late last year, when he was still confined to a forensic ward of Eastern State Hospital in Medical Lake, Washington. The legal challenge, he says, gives those patients “a grain of hope that they’ll be able to leave this place and start their lives over.” Still, Ross committed violence against two innocent senior citizens. Even if we accept the notion that he was not in his right mind and therefore not criminally responsible, how do we know he won’t do it again? “It’s not a fair question,” Ross responds. During more than an hour of conversation, it’s the only time his calm, rational voice takes on a note of urgency. “People get out of prison every day. They have a 65 percent recidivism rate compared to ours, which is 0.6 percent. The average citizen is as likely to commit a crime as a patient in the forensic ward of this hospital. It’s a 99.4 percent chance that I won’t.” The 2014 consultants’ report to the Washington State Department of Social and Health Services bears out Ross’s statistics, adding that insanity acquittees who are discharged commit less violence than the general population. While nationwide statistics don’t exist, the available Washington state data show acquittee violence rates ranging from 0 percent to 0.5 percent in recent years, according to Neil Gowensmith, an author of the report and a psychology professor at the University of Denver. By contrast, the overall national rate of violent crime in 2013 was 2.3 percent, a historic low. Numbers aside, “I don’t have to prove that I’ll never, ever, ever, ever, ever commit any, any, any criminal act,” Ross declares, “because I’m still a citizen of this country.” His suit invokes the rights to due process and equal protection set out in the 14th Amendment to the US Constitution. Raised mostly in Pullman—south of Spokane and home of Washington State University—Ross decided by age 16 that he wanted to become a civil rights attorney and, eventually, a Supreme Court justice. After graduating from Colorado College, he enrolled at Yale Law School in the fall of 2000. That first year was “disillusioning,” Ross recalls. “I had all these grand aspirations of using the law to achieve all these social justice goals.” But as he learned about the American legal system, “it became clear pretty quickly that it was going to be a much more difficult row to hoe. I was really angry, hurt, like the world was cheating me out of something.” Ross fell into a suicidal depression. He sought help from Yale Health, but he says they put him on a months-long waiting list, by which time the crisis had passed. (Asked for Yale Health’s response, a Yale spokeswoman says that by law, Yale Health officials cannot comment on patients’ medical histories.) That first year, Ross says, he didn’t experience symptoms of schizophrenia. But his friend and classmate Elisabeth Steele Hutchison ’03JD recalls a dinner conversation in which he told her that the State Department had hatched AIDS to infect African Americans. “I remember being taken aback, really surprised and off-put,” says Steele Hutchison, who is now admissions director at the University of Hawaii law school. “I always admired him. He’s so smart.” But his AIDS comment caused her to back away from the friendship. When he disappeared the next fall, she assumed he had transferred to another law school. Instead, Ross had decided that “I didn’t want to be an attorney, didn’t want to be at Yale,” he relates. “In my defiant mood” and suffering from paranoia, delusions, and hallucinations, he believed the CIA was after him because of his political activism. After leaving Yale, he “bounced around from place to place”—his father’s, his mother’s, Thailand—entangled in drugs, alcohol, “bad relationships, the whole nine yards.” He got in fights and cycled in and out of psych wards. With a diagnosis of schizoaffective disorder—later changed to chronic paranoid schizophrenia—he would take his medications for a week or two after leaving the hospital, then stop because he considered medication an admission of weakness. In 2007, Ross returned to Pullman “to make a new start. I thought I’d be facing my demons.” But it didn’t work. “My delusions about the CIA were really strong. I thought my next-door neighbors were traitors” and that the president was ordering him to get rid of them. He doesn’t like to talk about the assault, referring me to an account in the Inlander, a Spokane weekly that has written extensively about Ross and other patients found not guilty by reason of insanity. It says that he broke into his neighbors’ apartment, “stark naked and deeply psychotic, and hit them repeatedly with a broken broom handle.” “If he didn’t listen to the things he heard, he believed he’d be killed,” the Inlander continues. “He left five minutes later, his neighbors bruised and beaten, but alive.” Ross called the police himself, the Inlander reports. But even after his arrest, Ross says now, “I thought Army Rangers would break me out of jail.” It took about a month and a half in the county jail, under consistent medication, before his delusions became clear to him. “To this day it’s very difficult” to think about what he did, Ross says by phone. “You go from feeling really good about yourself to feeling really bad about yourself in a heartbeat. For me, that heartbeat was going from thinking I was a secret agent to realizing that I had assaulted my elderly neighbors.” That’s why he doesn’t regret using the insanity defense instead of accepting a plea bargain: without hospitalization and treatment, there’s no knowing what would have happened. “Would I have taken a life? Committed rape?” Don’t look for Ross to praise the hospital, however. Within six months or a year, “my treatment records started to reflect the fact that I’d stabilized on medications,” he says. “You would think that the hospital would take that and say, ‘OK, this person’s probably ready for release.’ But the hospital doesn’t care about recovery as much as you would think.” (A hospital spokesman, citing patient confidentiality laws, says he can’t comment.)  Matt LeitholtIf Ross had accepted a plea bargain and gone to prison, he says, he would have been detained for much less time. But he didn't regret it, because in the hospital he received treatment. View full imageRoss and Biviano trace Washington State’s high anxiety about patients who pleaded not guilty by reason of insanity—known as NGRI—to an incident in 2009: an NGRI patient from Eastern State Hospital walked away from a supervised outing at a county fair. He wanted to go home. After a three-day manhunt, the patient was captured. No one was hurt. But 22 years earlier, the man had killed an elderly woman during a psychotic episode. Although the hospital CEO called him “a fairly model patient,” his escape and his earlier violence caused panic branded him a “homicidal loon.” The next year, the legislature passed laws cracking down on NGRI patients. Before, patients who were stable could leave the hospital for supervised trips to stores, parks, and ball games. Now they need to apply for a court order just to leave the locked forensic ward and go outside. Each additional step toward freedom—permission to visit an ill family member; conditional discharge; final discharge—requires a separate court order, each typically executed at least six months after the previous request. Each step also requires a recommendation from a “public safety review panel,” on which mental health professionals are outnumbered by representatives of law enforcement, corrections, and prosecutors. The law had immediate consequences for many patients, including Ketema Ross, who had “substantially recovered” from his symptoms and “consistently demonstrated fully responsible behavior” on hospital outings, the lawsuit says. It adds that he lost all of his community privileges, which were integral to his treatment plan.  Matt LeitholtIn the lawsuit, Ross and his attorney argue that the state's restrictions hinder patients' recovery and deprive them of “dignity, respect, and worth.” View full image“The citizens of Washington are now safer,” state representative Matt Shea declared after the 2010 legislation passed unanimously. Calling the escaped patient “a dangerous and violent man who… should have never been taken out of the mental hospital,” Shea said: “This legislation is meant to ensure that dangerous forensic patients remain separated from the public except under very specific circumstances,” such as medical emergencies. In their 2014 report to the state’s Department of Social and Health Services, Gowensmith and other consulting psychologists call Washington “clearly an outlier” in its approach to NGRI acquittees. “Such lengthy hospitalization is unnecessarily expensive and restrictive,” the report continues. “The goals of public safety, financial stewardship, and patient recovery would all be better achieved by inpatient treatment that is briefer but more specialized.” Howard Zonana, cofounder and director of the Yale School of Medicine’s Law and Psychiatry Division and an expert on the insanity defense, doesn’t see Washington as an outlier: “Different states handle it differently.” Yale’s home state, for instance, is “more conservative” than Washington, with insanity acquittees held for an average of 15 years. (“You have to be crazy to plead insanity in Connecticut,” he half-jokes.) “Are we keeping people longer than they need to be?” Zonana asks. “Probably yes.” But even actuarial models produce only “moderate” success—about 75 percent, nationally—in predicting whether patients are safe and ready for discharge. “For the acquittee, [confinement] still feels like a punishment,” Zonana says. But “it is a choice” they make by pleading insanity. In their lawsuit, Ross and Biviano argue that Washington State’s restrictions are “devastating to patients,” hindering their recovery and depriving them of “dignity, respect, and worth.” They say the state law violates the Americans With Disabilities Act, as well as the constitutional rights to equal protection, minimally adequate treatment, and freedom from ex post facto punishment. In legal filings, Washington State responds that its treatment of NGRI patients is appropriate and legal: “Treatment professionals… exercise care and consideration when evaluating patients for a change in level,” which determines their privileges and restrictions. Far from being arbitrary, “a patient’s progress through treatment largely depends on that patient’s behaviors, motivation, and other factors within the patient’s control.” Under the current system, patients are “able to seek further privileges and freedoms, up to and including full discharge,” through the state courts, without intervention by the federal judiciary—and Ross has done so, the state notes. The Washington attorney general’s office declines to comment further. In October, a federal judge denied Ross’s motion for a preliminary injunction, saying he hadn’t provided enough evidence that the state court procedures are unconstitutionally slow and burdensome. Using those procedures, another plaintiff won final discharge last year—a development Biviano attributes to the suit. “We feel like it has definitely had an impact and has been worth the effort,” he says in an e-mail. He says they’re now negotiating in an effort to settle. Elisabeth Steele Hutchison met Ketema Ross 15 years ago, at a Yale Law School event for people of color who’d been admitted and were considering whether to enroll. They formed an “instant connection,” she says, but lost touch when he withdrew. Then last year, a Law School classmate committed suicide, and Steele Hutchison was asked to let other class members know. She tracked Ross down on Facebook, sent him a message, and eventually heard back from him—with a link to the Inlander article about him. It was the first she knew about the turn Ross’s life had taken. They reconnected by phone. She told him that she had developed depression during her first year at the Law School, was misdiagnosed, and spent years struggling with mental illness. “What struck me as so sad was: [our classmate] was suffering, I was suffering, Ketema was suffering, and we couldn’t talk about it,” Steele Hutchison says. “We could talk about racism, but we just didn’t have the vocabulary” to talk about mental illness. Asked why, she says: “Oh, stigma. Nobody says ‘Hi, I’m so-and-so and I suffer from major depression.’ I kind of think this is the next civil rights issue. We’ve kind of gotten through race, sexual orientation, gender—we haven’t solved any of them” but have made progress. Mental illness, she believes, will remain taboo until more people “come out of the closet” and disclose their personal struggles. “What Ketema’s done, which is so brave, is say, ‘This is who I am, and I am getting the care that I need to get,’” Steele Hutchison says. “This is a difficult path. I wouldn’t recommend it to him. I work at a law school now, and I said, ‘What are you doing?’” To which Ross responds: “Transparency’s kind of become a way of life for me. I really don’t have too much to hide. If people want to judge me by it, they will. If they want to give me a chance, they will.” More than 18 percent of US adults—43.7 million people—suffered from mental illness in 2012, according to the National Institute of Mental Health. Nearly 10 million had what is considered serious mental illness. The statistics are also sobering at Yale Law School: in a recent survey, 70 percent of students said they face mental health challenges. (The survey defined “mental health challenges” more broadly than the NIMH’s criteria for “mental illness.”) In addition, many say they can’t find the treatment or support they need. “We care deeply about the health and well-being of our students,” associate law dean Kathleen Overly responded by e-mail. “We are in the process of studying the report and will continue to work closely with our students on these critical issues.” In his first weeks out of the hospital, Ketema Ross found an apartment in Spokane, set up a bank account, bought groceries and pots and pans—“just the little things that people take for granted, but I certainly don’t at this point.” He quickly connected with a local clinic, where he gets psychiatric care, therapy, and medication. Because his hospital discharge is conditional, “there’s a whole list of conditions that I have to abide by,” he says: no firearms, no drugs or alcohol, regular check-ins, random drug testing. In a few months he’ll be eligible to go back to court and request final discharge. In the near future, he hopes for a job as a certified peer counselor, working with mental health patients in the community. In the longer term, Ross will probably apply to law school next year, perhaps at Gonzaga. But he’s uncertain about his plans: “I want to figure out where I can have the most benefit for mental health advocacy.” Meanwhile, he has already moved to a bigger apartment in a quieter neighborhood and started working out at the YMCA. After seven years of confinement, the biggest adjustment is simply being in charge of his own schedule and whereabouts. “It sounds kind of boring,” Ross says in describing his new life. “But believe me, I don’t mind.”
|
|
1 comment
-

Julie Bean , 9:19pm May 19 2015 |  Flag as inappropriate
Flag as inappropriate
The comment period has expired.Good article, but I have to note that the writer, perhaps unconsciously, went where she need not have gone. I2th paragraph. I have never heard a lawyer's or law student's averring with "urgency" (perhaps even "zealousness") contrasted against speaking in a calm or rational voice. Never seen the contrast re a non lawyer's speech. Goes to show that even those of us with the best intentions get sucked into wrong thinking.